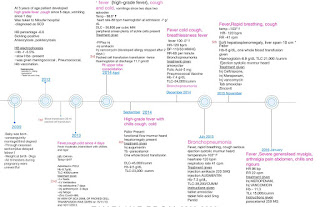
40Y OLD WITH CAP with Z positive
2024 JAN
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Patient and his/her attenders have been informed and their consent has been taken.
40 Y M WITH CAP
HOPI :
Patient came with complaints of cough since 10 days non productive
Complaint of SOB since 10 days MMRC grade 2, not associated with wheeze, aggravated in exertion and relieved on rest
No complaint of fever, chest pain,palpitations, orthopnea, hemoptysis
PAST HISTORY
Not a k/c/o DM, HTN, ASTHMA, TB, Epilepsy, CAD, CVA
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Sleep - Normal
Bowel and bladder movements -regular
No known allergies
Addictions Alcoholic occasional toddy 90ml
GENERAL EXAMINATION
Patient is conscious, coherent, cooperative
No pallor, icterus, cyanosis, clubbing, lymphadenopathy
Temp: 98.6°F
PR- 78bpm
RR- 17cpm
BP- 100/70 mmHg
Spo2 -97%at RA
Grbs- 103mg/dl
SYSTEMIC EXAMINATION
CVS S1 S2heard no murmurs
RS - BAE, NVBS heard, Crepts over bilateral IAA, ISA
P/A - Soft, non tender
CNS- NFND
INVESTIGATION
Retroviral positive
Sputum for AFB negative, no pathogenic organism isolated on culture.
DIAGNOSIS
Retroviral positive denovo with Community Acquired Pneumonia ? TB
Anaemia (Microcytic Hypochromic) with Bicytopenia








Comments
Post a Comment