70 Year old Female with Shortness of breath
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This Elog book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment .
5 Dec
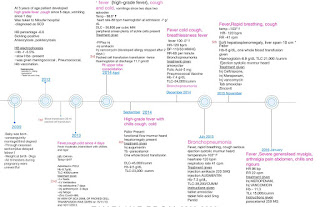
70 year old female Resident of Vemulapalli
Housewife
Chief complaints of Shortness of breath since 10days
Decreased appetite since 4 days
Weakness since 4 days
History of Presenting Illness
Patient was apparently asymptomatic 5 years back then she developed Shortness of breath and was taken to private hospital was treated with Nebulization , Diagnosed as Bronchial Asthma and was on medication since then.
Shortness of breath seasonal variation ( every year during winters)
Patient developed similar complaints with fever and was admitted in Private hospital was treated as Bronchial asthma 6 months back
10days back she developed Shortness of breath grade MMRC grade 3 which was insidious in onset and gradually gradually progressive. Complaint of cough non productive, fever.
Not associated with chestpain , Palpitations, sweating
No history of orthopnea , paroxysmal nocturnal dyspnea.
Symptoms were relived in giving medication Nebulization
4 days back patient developed increased shortness of breath MMRC grade 4 , weakness , increased fatigue, decreased appetite, unable to move from bed or walk without support
Yesterday patient was taken to miryalaguda hospital with Complaint of shortness of breath and unable to swallow more for solids .
Evaluation was done and referred to our hospital
Past History
10 years back patient had history of fall (head injury) which was not associated with loss of consciousness, projectile vomiting , seizure, weakness of limbs
Nueroimaging of brain was done
She was diagnosed with Hypertension and was started on medication.
Patient was diagnosed with hypothyroidism
since 4 years
Not a known case of DM, Tuberculosis ,epilepsy
Family History
Not significant
Personal History
Diet Vegetarian
Appetite Decreased
Sleep adequate
Bowel and bladder movements regular
No addictions and allergies to pollen dust
Daily routine
She wakes up in morning
Eats 3 times
Walks around the house or sleeps
General Examination
Patient is conscious
Thin built and malnourished
Pallor
No Icterus, Clubbing, cyanosis,lymhadenopathy, pedal edema
Vitals
At presentation
GCS E4V5M6
RR Tachypniec
BP 110/70 mm Hg
PR 120bpm irregular
SpO2 89%on Room air and 96% on 2litres of O2
GRBS 141mg/dl
ECG
Currently
Temp: afebrile
PR- 110 beats/min
RR- 27 cpm
BP- 100/60 mmHg
SpO2 98% on 3litresO2
SYSTEMIC EXAMINATION
RS-
Inspection
Shape of chest elliptical
Bilateral chest symmetrical
Equal chest expansion on both sides
Thoracoabdominal type
Trachea appears to be central
Supraclavicular hollow present
Right
No muscle retraction, grunting, crowding of ribs
Palpation-
All inspectory findings confirmed
No rise of temperature
No tenderness
Chest circumference 72 cm
Anterior posterior 20 cm
Transverse 32 cm
Ratio is 0.625 (5:8) (Normal is 5:7)
Trachea central
Symmetrical chest movements
Apex beat left 5th intercoastal space
Percussion-
Resonant in all areas
Resonant in Right 6th Intercoastal space Tidal percussion
Auscultation-
Bilateral air entry present
Crepitations at bilateral infra axillary area
Rhonchi at infra axillary and infra scapular area
CNS Examination
HMF intact
Oriented to time place and person
Motor
Tone Normal
Power 4/5 In all muscles
Reflexes Bilaterally
Biceps 2+
Triceps 2+
Supinator 2+
Knee 2+
Ankle 2+
Plantar Flexion
Sensory system Intact Bilaterally Pain Temperature Touch and Pressure
CVS-
S1 S2 heard, no murmur
P/A -
Soft, non Tender, no organomegaly
Urine output
Investigations
4th Dec
Labs-
Hb- 10.1
Tlc- 18.5K
Plt- 3.32lks
Na- 123(dec)
K- 3.3(dec)
Cl- 82
Serum osm- 254(hypotonic)
Urinary Na- 125
K-26.9
Cl-149
Abg-
Ph- 7.54
PCo2- 27.8
PO2- 61.6
SpO2- 93.5
Hco3- 26.3(st) 23.8(c)
( metabolic alkalosis)
Provisional Diagnosis--
Acute exacerbation of Asthma?
Miliary TB?
ILD ? COPD ?
With Hyponatremia, hypokalemia under evaluation
Follow up
8th Dec
S
Fever spikes -
Stools Passed +
Skin pinch normal
Cough -
O
Patient is conscious, coherent, cooperative
Temp- 98.4 F
BP- 110/60 mmHg
PR- 78 bpm
RR- 20 cpm
SPO2- 93% on RA
GRBS- 130 mg/dL
CVS- S1, S2 +
RS
BAE +
Trachea- Central
Rt. Lt
Supraclavicular. Rhonchi. Clavicular
Clavicular. Crackles, crepts. Crepts, rhonchi
Infraclavicular. Rhonchi. Rhonchi
Mammary. Crepts. Crepts&Rhonchi
Axillary. Rhonchi. Crackles
Infra axillary. Rhonchi, crackles. Crackles
Inter scapular. Crackles. Crepts, rhonchi
Infra scapular.Crackles,crepts.Crackles, crepts
P/A- Soft, Non tender
CNS- HMF+
Hemogram
Hb- 7.5 mg/dL
TLC- 6700 cells/cumm
RBC- 2.98 millions/cumm
PLT- 2.59 lakhs/cumm
Serum electrolytes
Na+ 134 mEq/L
K+ 3.6 mEq/L
Cl- - 103 mEq/L
Ca2+ - 0.96 mmol/L
A
Acute exacerbation of ? Asthma ? COPD
? ILD ? Miliary TB ? CAP
With hyponatremia (Resolved) Hypokalemia (Resolving) (Hypovolemic)
with septic shock (Resolving)
HTN+ since 1 year (Under Tab. Telma H Stopped)
With hypothyroidism (Not under medication)
P
1. IVF NS @ 100 ml/hr
2. Inj. PIPTAZ 4.5 g IV/TID (Day 4)
3. Inj. Hydrocortisone 100 mg IV BD (Day 3)
4. Inj. PAN 40 mg IV OD BBF
5. Tab. Montek LC PO BD
6. Tab. Azithromycin 500 mh PO OD (Day 3)
7. Tab. Pulmo clear 100/600 PO BD
8. Syp. POTCHLOR 20 mEq (15 ml) in 1 glass water PO TID
9. Syp. Grillinctus 10 ml PO BD
10. Syp. Aristozyme 5 ml PO BD
11. Nebulization with
Ipratropium - 6th hrly (QID)
Budecort - 12th hrly (BD)
Mucomist- 12th hrly (BD)
12. O2 inhalation to maintain saturation >90%
13. Monitor vitals
14. Strict I/O charting
15. Inform SOS
9 Dec
10 Dec


























Comments
Post a Comment