80Y OLD MALE with QUADRIPLEGIA
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
4 Feb 2022
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This Elog book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment .
Patient and his/her attenders have been informed and their consent has been taken.
A 80Y OLD MALE CAME WITH CHIEF COMPLAINTS OF B/L UPPER AND LOWER LIMB WEAKNESS
HOPI
Patient was a shepherd. He stopped working 5 years ago on the advice of his family as he was getting tired very easily.
Since then, he stays at home all day and was able to look after himself in terms of brushing, bathing, feeding etc.
Patient had Fever which subsided on taking medicines.
3 days ago: Patient had his dinner around 8 pm and went to bed. At around 10 pm he then suddenly fell off the bed and complained of neck pain and inability to use both his upper and lower limbs. He was taken to the local RMP who checked his blood pressure and told him he was Denovo hypertensive. Unknown medication was given.
Since 2 days, the patient has slurring of speech and non productive cough.
Past history:
No similar episodes in the past.
Not a known case of diabetes mellitus, asthma, epilepsy, coronary artery disease.
No surgical or drug history
Personal history:
Mixed diet
Appetite is normal
Bowel and bladder are regular
Sleep is adequate.
He was an occasional toddy drinker, 90 mL during festivals. Stopped 5 years back. Does not smoke.
No known allergies.
Family history:
No similar complaints.
Patient is examined in a well lit room after obtaining informed consent. She is conscious, coherent and cooperative, well oriented to time, place and person, moderately built and nourished.
General Examination:
Pallor: Present
Icterus, cyanosis, clubbing, generalized lymphadenopathy or edema are not observed.
Vitals:
Temp.- Afebrile
BP- 190/100 mmHg
PR- 92 bpm
RR- 21 cpm
SpO2- 96%
GRBS- 144 mg/dL
CNS:
Higher mental functions:
Oriented to time,place,person
Memory : recent, remote intact
Speech: Not understandable
No delusions or hallucinations
Cranial nerves:
1- not tested
2- binocular vision: decreased in right eye due to senile immature cataract
3,4,6- No restriction of movement of eye
5-normal( muscles of mastication+sensations of face)
jaw jerk is present
7-Normal, wrinking of forehead seen, able to blow up cheeks
8- Normal hearing
9,10,11,12-normal. Gag reflex is normal.
Motor examination:
Tone - decreased in upper limbs, normal in lower limbs
Power
1/5 in lower limbs
0/5 in upper limbs
Reflexes :
Biceps: Right, left: absent
Triceps: B/l absent
Supinator: Right, left: absent
Knee: Right: 2+
Left: 3+
Ankle: Right: 1+
Left: 2+
Plantars: Flexion of leg at knee joint is seen. Mute
Sensory examination:
Deep pain is absent below nipple area
Cerebellum examination:
Able to do finger nose test.
No dysdiadokinesia
No rebound tenderness
Autonomic Nervous System:
No postural hypotension
No bladder and bowel incontinence
No sweating abnormalities
Meningeal sign Absent
Gait: did not walk due to weakness
CVS: S1 S2+ no murmurs heard.
Respiratory system- Bilateral air entry+ ,normal vesicular breath sounds-heard.
Abdominal: Soft, non tender, no distension, umbilicus is central and inverted.
INVESTIGATIONS:-
HEMOGRAM-
HB:- 8.3GM/DL
TC:- 5,300
N/L/E /M :- 95/ 02/01/02
PCV :- 25.6
MCV- 80.5
MCH:- 26.1
MCHC:- 32.4
RBC :- 3.18
PLATELETS:- 4.72
NORMOCYTIC NORMOCHROMIC ANEMIA WITH NEUTROPHILIC LEUCOCYTOSIS.
COMPLETE URINE EXAMINATION:-
PUS CELLS- 3-4
EPITHELIAL CELLS - 2-3
ALBUMIN:- TRACE (2.8)
SUGARS:- NIL
RBS- 162MG/DL
FBS:- 144MG/DL
PLBS:- 126MG/DL
LFT:-
TB:- 0.55
DB:- 0.18
AST:- 19
ALT:- 10
ALP:- 135
TOTAL PROTEIN:- 5.7
A/ G RATIO:- 0.96
RFT:-
BLOOD UREA -52
SERUM CREATININE - 0.9
Na:- 137
K:- 5.8
Cl:- 102
HBA1C:- 6.6 %
FASTING LIPID PROFILE:-
TOTAL CHOLESTROL:- 112MG/DL
TRIGLYCERIDES:- 174 MG/DL
HDL CHOLESTEROL:- 30MG/DL
LDL CHOLESTROL:- 89 MG/DL
VLDL:- 35MG/DL
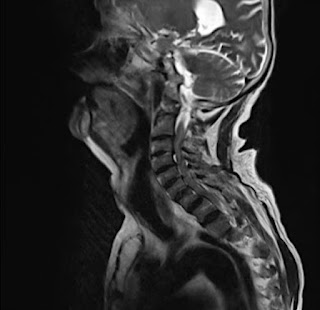
MRI:
IMPRESSION:-
1) MODERATE TO SEVERE CERVICAL SPONDYLOSIS AT MULTILEVEL C2-C3 , C3-C4 , C4-C5 & C5-C6 LEVEL WITH COMPRESSIVE MYELOPATHY CHANGES AND SPINAL CANAL STENOSIS
2) NEURAL IMPRINGEMENT AT C4-C5 , C5-C6 LEVELS.
USG report
Bilateral Grade 2 Renal Parenchymal Disease with Simple cortical cyst.
Chest: Mild pleural effusion on right
Mild pleural effusion on left with Consolidation in peripheral lung parenchyma
Doppler:
Ejection Fraction:- 48%
Mild LV dysfunction
Mild diastolic dysfunction ,
Mild PAH
DILATED RA / LA/ RVH
PROVISIONAL DIAGNOSIS
? Compressive myelopathy
Treatment:
1) IV FLUIDS @75 ml/hr
2) CERVICAL HARD COLLAR
3) TAB AMLONG 5MG PO/OD
4) TAB PAN 40MG PO/OD
5) TAB ZOFER 4MG PO/ SOS
6) BP/ PR/ RR / TEMP CHARTING
7) STRICT IPO CHARTING
8) INJ OPTINEURON 1 AMP IN 100ML NS / IV / OD
Pleural tap was advised.








Comments
Post a Comment